Which way is the best, and how, to cure Hemorrhoids?
Evidence-Based Insights and Personal Experiences for effective Hemorrhoid Management.
I hope you have been well over the last couple of weeks, and the coming US Elections next week are not praying too heavily on your mind. Half-term this week in the UK means looking after my kids full-time, which has been challenging with a little toddler, but brought us together more. This week, ready in time for Halloween tomorrow, here’s my horror(!) story!
Word Count: 3014
Reading Time: 12 mins 40 secs.
I’m just going to come out and say it because there isn’t a nice way of saying it. I was in the shower, and had an itchy bottom and when I felt behind down there, I could feel a tiny squishy bulb, at the opening of my anus that I couldn’t wash away, however much soap I used. It wasn’t painful to touch but it was weird, and I wondered if it was normal?
First off, I’m not the only one, apparently. Over half of men and women over 50 in the US have hemorrhoids[1], so it is actually pretty normal. Flip a coin at my age and the chances are, if it comes up tails(!) you have it. But why? And how the heck did it get there?
If you are anyone like me, you might be asking yourself the same question, but too afraid to ask anyone else. It isn’t something you are likely to discuss over coffee or at the water cooler at work, ‘Hey, you’re not going to believe this, last night I stuck my finger up my anus and…” So, this week, I am going to get to the bottom(!) of it, reviewing the latest research, which frighteningly suggests it may be caused by bacteria, some of which are resistant to antibiotics, and give my personal experience of what I did to cure it!
Key Findings
1) There are three theories of the cause of hemorrhoids: the varicose vein theory; the
vascular hyperplasia theory; and the theory of sliding anal canal lining.
2) A Sitz bath and Anusol relieved my symptoms of Stage 1-2 hemorrhoids.
3) Lifestyle changes including a high-fibre diet and water intake helped me to heal.
4) A squat toilet adaptation may aid defecation more naturally in line with the colon.
5) There are 4 grades of hemorrhoids and rubber band ligation is recommended for Stage 2.
1. What even are hemorrhoids?
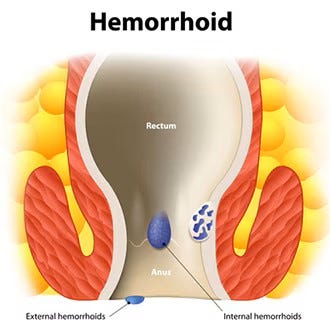
Hemorrhoids, or piles, are “swollen and inflamed veins around your anus or in your lower rectum.”[2] Also known as “varicose veins of the anus and rectum”. They occur when the blood vessels stretch and bulge. As these vessels expand, their walls become thinner, similar to a balloon that's been inflated too much, which can lead to bleeding if they break. If the pressure and stretching continue, these weakened vessels may protrude, causing itchiness, which is a symptom, as well as discomfort or pain defecating.
There are two types, external, under the skin around the anus, and internal, in the lining of the anus or lower rectum (see pic below).
What I thought I had was external hemorrhoids, because it was just at the entrance of the anus, which is lucky, because if it is internal, you’re going to need a doctor to gel up a rubber-gloved finger to diagnose it.
I know, because it got worse, and I found it incredibly painful to defecate at one point, and there was blood when I wiped my bottom, and had the procedure to check. Afterwards, when I moaned about the discomfort of the procedure, the doctor said, “Imagine how I feel!” Quite.
2. So what causes hemorrhoids?
When I asked the doctor, he scrunched up his face to express strain and simulated pushing a stool.
What he should have said was this:
“In the medical field, there is no consensus on the etiology of hemorrhoids. Currently, there are several main theories on the causes of hemorrhoids: (1) the varicose vein theory, (2) the vascular hyperplasia theory, and (3) the theory of sliding anal canal lining, which is widely accepted (Palumbo et al., 2023). The earliest theory proposed that hemorrhoids may be related to varicose veins, such as varicose swelling caused by increased local pressure from hard stools (Burkitt, 1972; Chawla and Dilawari, 1989). Some scholars believe that the formation of hemorrhoids may be a result of vascular proliferation during the inflammatory response and tissue remodeling process (Chung et al., 2004; Aigner et al., 2009). The latest theory suggests that the pathological sliding of the anal cushions is the main cause of hemorrhoid formation (Thomson, 1975; Haas etal., 1984; Loder et al., 1994; Lohsiriwat, 2012). The above three theories are based on the characteristics of human tissues. In addition to the reasons mentioned above, dietary habits such as a low-fibre diet, lack of regular exercise, and low water intake are also believed to be associated with the formation of hemorrhoids (Feyen et al., 2022).” [3]
Although, most of the online guides I found did suggest “strain during bowel movement” was a cause, among the following:
Straining during bowel movements.
Sitting on the toilet for long periods of time.
Chronic constipation or diarrhea.
A low-fiber diet.
Weakening of the supporting tissues in your anus and rectum. This can happen with aging and pregnancy.
Frequently lifting heavy objects.[4]
But I confirmed this with a study which explained that “forced and prolonged straining during defecation, and the adverse effect on lymphatic circulation” may cause an anal edema to develop.[5]
What I didn’t know was that too much cleaning around your anus may make the symptoms worse. The irony of my shower. Go figure!
The good news is that external hemorrhoids can go away on their own within a few days. Internal hemorrhoids are not usually painful, unless they prolapse, which means it has fallen through your anal opening, which is what had happened to me.
3. How did I treat my own hemorrhoids?
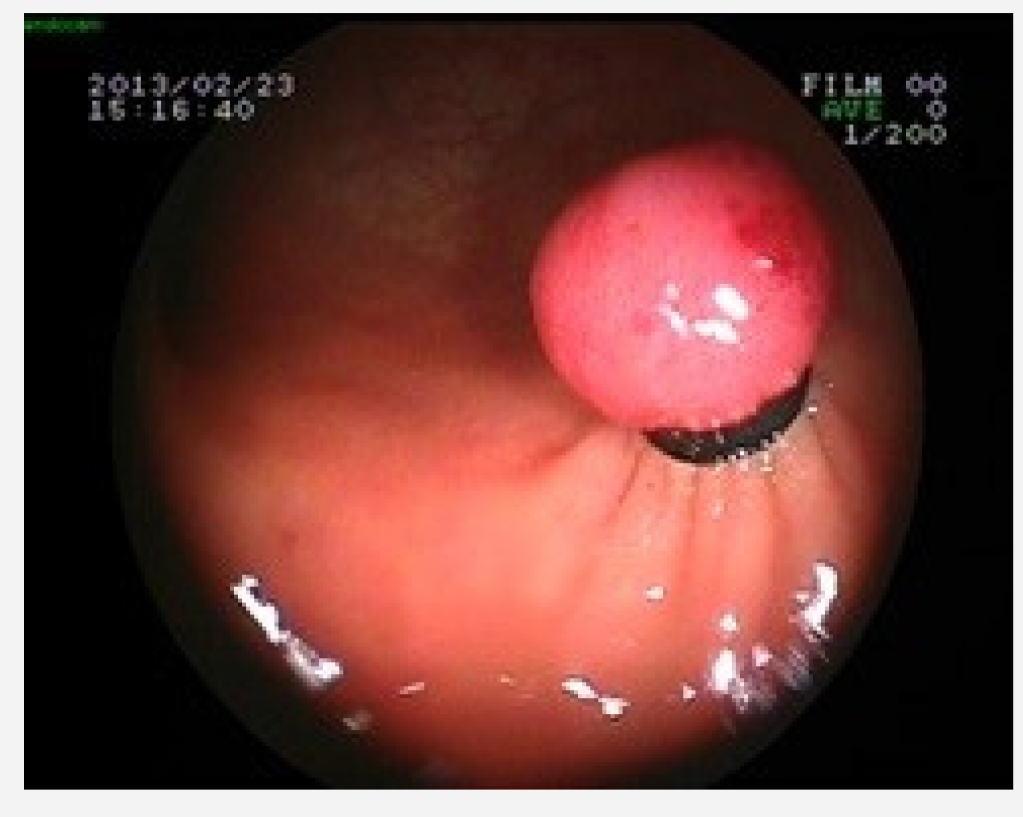
Warning: Contains medical pictures which some may find upsetting.
First, I was told to take a warm bath a few times a day, and I was amazed that this actually made a difference. You can also have a sitz bath using one of these on your toilet and pour warm water into it:
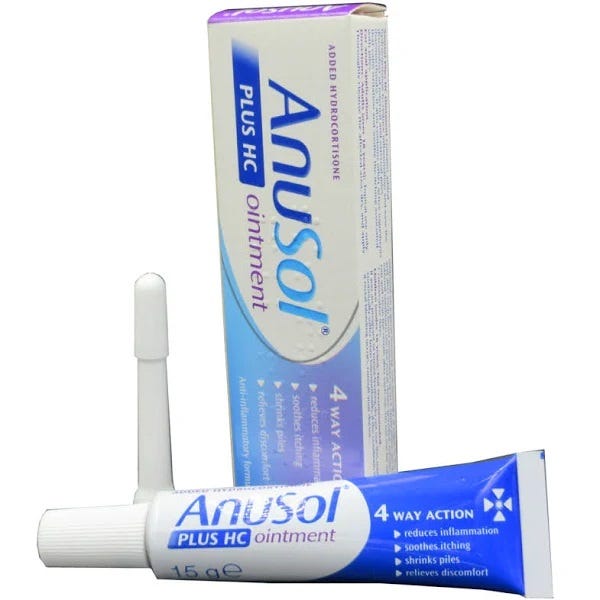
But I found sitting in a shallow hot bath for 10 to 20 minutes, a few times a day, helped the healing process and was enough to relieve my symptoms with the ointment I was given, Anusol, which contains zinc oxide, bismuth oxide and balsam peru, and comes with a nozzle you can use to insert internally.
I used it after a hot bath, and drying the anus gently, and this stuff was amazing, although it may be psychological. You can buy it online without a prescription. However, I am not medically qualified, and I highly recommend visiting your doctor, like I did, before using any medication, because there may be other complications.
“Over the counter hemorrhoid creams and suppositories may provide temporary relief for some but do nothing to help reduce the increased pressure in the rectum… Their usage may also mask symptoms due to other conditions such as colorectal or anal cancer. It is not safe to assume your bleeding, pain, or itching is due to hemorrhoids.”[6]
However, the Hemorrhoid Centers of America, which are not sponsoring this post, also state, “Steroids and OTC preparations or suppositories are ineffective and do not help the increased anal pressure and pain,” but, for me, Anusol helped, but importantly, with a change in diet.
4. How does diet affect hemorrhoids?
I found I was straining to defecate because I was constipated, and my stools were too hard. This may be because I wasn’t drinking enough water and not eating enough fiber. Although low fiber and constipation are commonly reported as a cause of hemorrhoids, this has not actually been proven.[7]
Another study found that diarrhea rather than constipation was associated with hemorrhoids.[8]
I can’t remember if I had diarrhea before, which may have developed the hemorrhoids, but not caused a notable pain, and constipation may have simply exacerbated it.
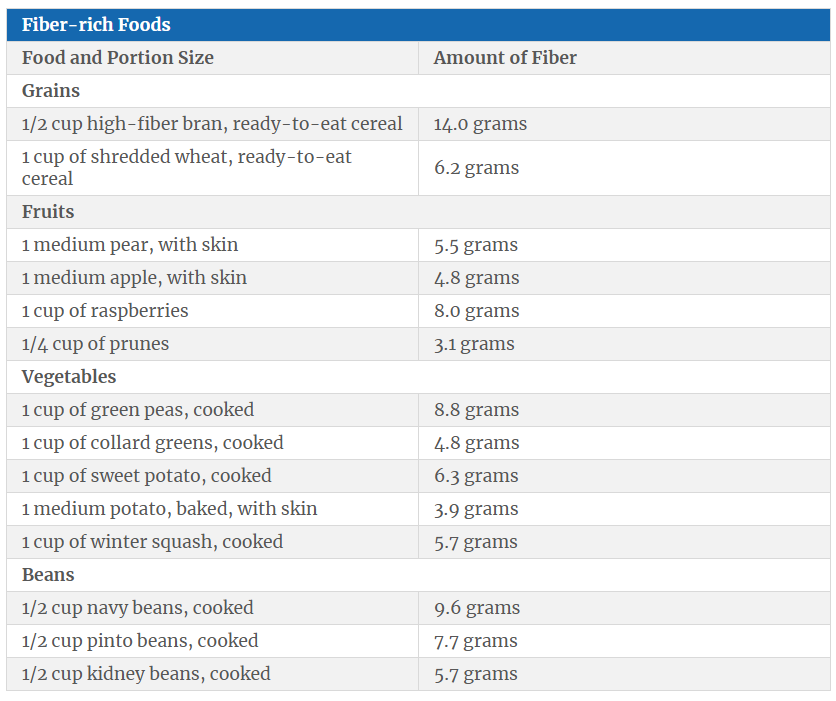
However, avoiding constipation definitely helped me with hemorrhoids, and eating a higher fiber diet of, depending on age and sex, between 22 to 34 grams of fiber a day[9] will make stools soft, formed and bulky, and the table below which shows how much fiber is in different foods, may help.
“First-line therapy typically involves dietary modification with adequate fluid and fibre intake, along with avoiding straining and limiting prolonged time on the toilet.”[10]
The foods to avoid[11] if you have hemorrhoids, with little or no fiber include:
cheese
chips
fast food
ice cream
meat
prepared foods, such as some frozen and snack foods
processed foods, such as hot dogs and some microwavable dinner
Also, having enough water, approximately 2 and a half litres a day for my size (see Whichwayhow to cure Nocturia (without medication) here) helps the fiber in your diet work better and helps prevent hard stools and aid healing.
Another important tip is not to spend more than 3 to 5 minutes on the toilet [12]. You can always come back again if you still need to defecate.
And do not sit for more than 2 to 3 hours in a chair. Get up and have a break, walk around, exercise is good for you.
And interestingly, hemorrhoids are more common in the Western hemisphere, and it has been proposed that this is because squatting on the toilet is healthier because it opens the kink in the colon (see pic below).
You can find many devices on Amazon to help accomplish this, like this one for £12.99:

If you can, avoid alcohol, which is known to cause dehydration, and if you are struggling with alcohol, you can get help to control or quit drinking in my book here.
Another study I read, made me wonder again about the link between diarrhea and hemorrhoids because it explained that research suggested microbes play a role in the development of hemorrhoids. It analyzed 49 different bacterial strains from seven patients with hemorrhoids. The study focused on special structures within bacteria called plasmids, some of which contained genes that make bacteria resistant to antibiotics, which makes treating infections even more difficult.[13]
However, while diarrhea may have a viral or bacterial etiology, another study showed that it wasn’t gut microbes, but rather skin microbes, specifically Staphylococcus, which are “more abundant on hemorrhoid surfaces”.[14]
There is much exciting research in this field underway, but I can confidently say already, there may be more to it than over-straining when you defecate, like my doctor said!
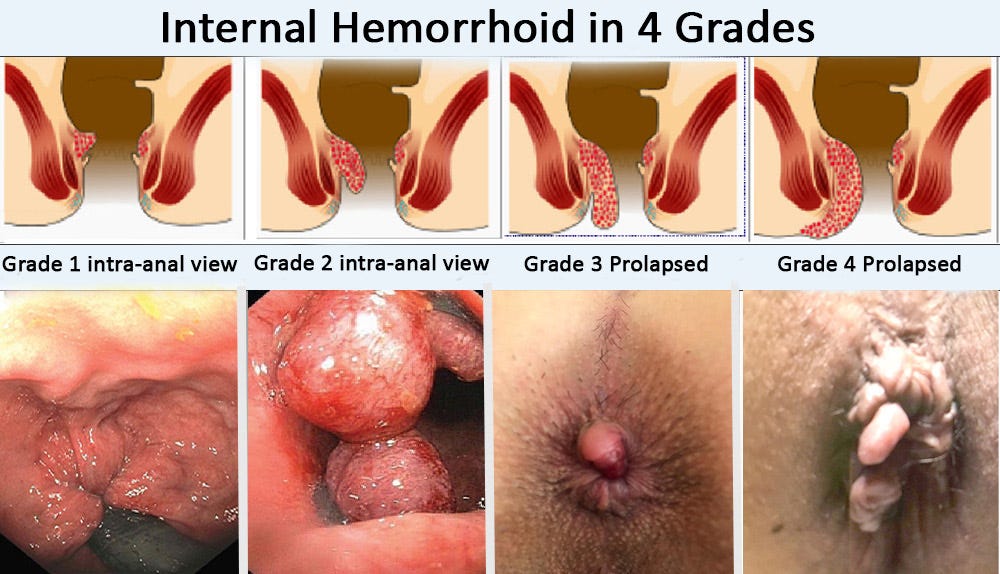
5. What are the different grades of Hemorrhoidal disease?
“Hemorrhoidal disease is divided into four grades according to Goligher [11]. In grade one, proctoscopy shows slight bulging of the hemorrhoids. In grade two, the hemorrhoids prolapse into the anal canal on defecation with spontaneous reduction. In the case of grade three hemorrhoids, the prolapsed hemorrhoids protrude outside the anal canal and do not spontaneously reduce but can be manually repositioned. Grade four hemorrhoids are irreducible and constantly prolapsed.”[15]
In more severe cases at Grade 3 or 4, you may require surgery, which is called a hemorrhoidectomy.
However, I had grade 1 or 2 hemorrhoids, which my doctor said didn’t require surgery. Although, in grade 2 hemorrhoids, rubber band ligation is recommended. “The hemorrhoid tissue is tied off at the base with a rubber band. The tissue dies and falls off. The resulting scarring results in repair of the remaining hemorrhoid tissue.”[16]

The Hemorrhoid Centers of America offers this non-surgical banding treatment which they call a “Disposable Hemorrhoid Ligation System” and describe how the procedure works here:
“Our ligation system uses a sterile, disposable device to apply gentle suction to the problem area, with the physician then placing a small rubber band over one internal hemorrhoid. The rubber band cuts off the blood supply to the hemorrhoid, reducing its size and pressure. The band may fall off as soon as 48 hours after the banding. There are usually three banding sessions required at two week intervals.”[18]
Like I said, I didn’t require this procedure, but if you have been diagnosed with stage 2 hemorrhoids this is the best procedure I have found, rather than laser, cutting off, or injecting the hemorrhoids, which come with greater risks, although may be necessary with higher stage hemorrhoids.
6. Conclusion
There is nothing to be ashamed of about having hemorrhoids. It is common in pregnancy and in the over-fifties.
In this article I have even explained that it may not be something you caused yourself by over-straining when you defecate, but have a microbiomial etiology, contrary to what my doctor suggested! Don’t believe everything doctors say, like I explained, the jury is still out on the cause!
However, it is important to get it checked out by a doctor at the earliest opportunity, because as I found to my horror, it can become worse if it doesn’t go away in a few days, and there may be underlying complications. I described the procedure in a slightly comical way, but it isn’t that bad, and you just have to grin and bear it, you imagine it a lot worse than it is, and it is over in seconds.
I do think diet makes a difference, though, in my personal experience. Water, with a touch of salt (salt may be better for you than you think) and enough fiber in your diet (see Whichwayhow Atkins, coming soon! If you are on an Atkins diet) are important, and go easy on alcohol. The recommended amount is a glass of wine a day, as a rough guide, although I don’t believe there is any ‘good’ amount of a poison!
With these behavioural changes, coupled by warm baths and a cream for relief, I was able to successfully treat Stage 1 to 2 hemorrhoids myself.
So, next time you’re at the water cooler, and someone complains of an itchy bottom, be nice, and don’t assume they don’t use enough toilet paper!
Bonus Tip:
As a bonus for reading to the end, I’ll give you another tip: Wipe your bottom with toilet paper three times. No more. If you still feel dirty, have a shower. If you constantly wipe more than this you are just aggravating the skin, with ever-decreasing efficiency at cleanliness, and making things potentially worse!
If you’d like to buy me a coffee you can do so below:
Please share this article to help others:
And if you don’t want to miss the next deep dive in a fortnight—which may be just what you need to solve your problem—subscribe for FREE below (No paid option, Whichwayhow.com is always free!)
References
[1] Fox A, Tietze PH, Ramakrishnan K. Anorectal conditions: hemorrhoids. FP Essentials. 2014;419:11–19.
[2] https://www.niddk.nih.gov/health-information/digestive-diseases/hemorrhoids Accessed at 10:14 on 28th October 2024.
[3] Wang YQ, Su W, Liu Z, Wang YH, Li L, Xu H, Wang M and Shen W (2024) The microbiomic signature of hemorrhoids and comparison with associated microbiomes. Front. Microbiol. 15:1329976. doi: 10.3389/fmicb.2024.1329976
[4] https://medlineplus.gov/hemorrhoids.html Accessed at 10:29 on 28th October 2024.
[5] GÜLEN, M., EMRAL, A.C., EGE, B. (2024). Management of Hemorrhoid Rubber Band Ligation Complications: Massive Rectal Bleeding. Namık Kemal Medical Journal, 12(1), 40-44. doi:10.4274/nkmj.galenos.2023.36036.
[6] https://hemorrhoidcentersamerica.com/hemorrhoids/ Accessed at 11:36 on 28th October 2024.
[7] Sandler RS, Peery AF. Rethinking What We Know About Hemorrhoids. Clin Gastroenterol Hepatol. 2019 Jan;17(1):8-15. doi: 10.1016/j.cgh.2018.03.020. Epub 2018 Mar 27. PMID: 29601902; PMCID: PMC7075634.
[8] Johanson JF, Sonnenberg A. Constipation is not a risk factor for hemorrhoids: a case-control study of potential etiological agents. Am J Gastroenterol 1994;89:1981–6.
[9] U.S. Department of Agriculture and U.S. Department of Health and Human Services. Dietary Guidelines for Americans, 2015–2020. 9th Ed. Published December 2020.
[10] Sandler RS, Peery AF. Rethinking What We Know About Hemorrhoids. Clin Gastroenterol Hepatol. 2019 Jan;17(1):8-15. doi: 10.1016/j.cgh.2018.03.020. Epub 2018 Mar 27. PMID: 29601902; PMCID: PMC7075634. See also, Alonso-Coello P, Mills E, Heels-Ansdell D, et al. Fiber for the treatment of hemorrhoids complications: A systematic review and meta-analysis. The American Journal of Gastroenterology 2006;101:181–188. [DOI] [PubMed]
[11] https://www.niddk.nih.gov/health-information/digestive-diseases/hemorrhoids/eating-diet-nutrition
[12] Jacobs DO. Hemorrhoids: what are the options in 2018? Curr Opin Gastroenterol 2018;34:46–49. [DOI] [PubMed]
[13] Wang Y, Su W, Zeng X, Liu Z, Zhu J, Wang M, Li L, Shen W. Surprising diversity of new plasmids in bacteria isolated from hemorrhoid patients. PeerJ. 2024 Aug 30;12:e18023. doi: 10.7717/peerj.18023. PMID: 39224828; PMCID: PMC11368089.
[14] Wang, Yuquan & Su, Wenya & Liu, Zhiqiang & Wang, Yihua & Li, Ling & Xu, Hai & Wang, Mingyu & Shen, Wenlong. (2024). The microbiomic signature of hemorrhoids and comparison with associated microbiomes. Frontiers in Microbiology. 15. 10.3389/fmicb.2024.1329976.
[15] Feyen L, Freyhardt P, Schott P et al. Hämorrhoidenembolisation: Eine neue minimalinvasive endovaskuläre Therapieoption bei Hämorrhoidalleiden. Fortschr Röntgenstr 2022; 194: 266 – 271https://www.thieme-connect.de/products/ejournals/html/10.1055/a-1662-5487?articleLanguage=en
[16] Feyen L, Freyhardt P, Schott P et al. Hämorrhoidenembolisation: Eine neue minimalinvasive endovaskuläre Therapieoption bei Hämorrhoidalleiden. Fortschr Röntgenstr 2022; 194: 266 – 271. See Also Paikos, Dimitrios & Gatopoulou, Anthia & Moschos, John & Koulaouzidis, Anastasios & Bhat, Sharanya & Tzilves, Dimitrios & Soufleris, Konstantinos & Tragiannidis, Dimitrios & Katsos, Ioannis & Tarpagos, Anestis. (2007). Banding hemorrhoids using the O'Regan Disposable Bander. Single center experience. Journal of gastrointestinal and liver diseases : JGLD. 16. 163-5.
[17] GÜLEN, M., EMRAL, A.C., EGE, B. (2024). Management of Hemorrhoid Rubber Band Ligation Complications: Massive Rectal Bleeding. Namık Kemal Medical Journal, 12(1), 40-44. doi:10.4274/nkmj.galenos.2023.36036.
[18] https://hemorrhoidcentersamerica.com/non-surgical-hemorrhoid-treatment/ Accessed at 11.48 on 28th October 2024.